急性心筋梗塞・大動脈解離手術後の胸の痛み、パニック障害に似た症状の考察

こんにちは。けんこうカイロプラクティックセンター(静岡市葵区) 代表カイロプラクター 岩崎久弥(いわざきひさや)です。今日のブログテーマは、「急性心筋梗塞・大動脈解離手術後の胸の痛み、パニック障害に似た症状の考察」

実は、私は急性心筋梗塞で、二度、緊急カテーテル手術を受けています。なので急性心筋梗塞後の心臓の辛さを一番良くわかっているカイロプラクターだと自負しています。こんなこと自負してもしかたないのですが、最近、急性心筋梗塞・大動脈解離手術をうけた方々からの相談が少しずつ増えているので、なんとかお役にたちたいと思い、ブログテーマに選択しました

Janet Graeme Travell (December 17, 1901 – August 1, 1997) was an American physician and medical researcher. Contents 1 Early life and education 2 Career 3 Research 4 Quote 5 References 6 External links Early life and education[edit] She was born in 1901 to John Willard and Janet Eliza (Davidson) Travell. Heavily influenced by her father’s profession of physician, Travell made the decision to pursue a career in the medical field. In June 1929, in New York City, Janet married John William Gordon Powell, who was an investment counselor. They had two daughters—Janet and Virginia. At the age of 95, Travell died of heart failure at her home in Northampton, Massachusetts. She is remembered as President John F. Kennedy’s personal physician and a researcher of the concept of trigger points as a cause of musculoskeletal referred pain. 彼女はジョン・F・ケネディ大統領の主治医であり、筋骨格関連痛の原因としてのトリガーポイントの概念の研究者として記憶されています。 Career During her career, Dr. Travell pioneered techniques for the treatment of myofascial pain, including dry needling. Her career began with her educational pursuits at Wellesley College and continued in graduate school as she pursued an M.D. from Cornell University Medical College in New York City. Upon graduating in 1926, Travell completed two years of residency at New York Hospital while concurrently serving as an ambulance surgeon for the New York City police force. After completion of residency, Travell became a research fellow at Bellevue Hospital, where she studied the effects of digitalis in patients with lobar pneumonia. Once her fellowship was concluded, Travell returned to Cornell University to serve as instructor in the Department of Pharmacology and later as Associate Professor of Clinical Pharmacology. While working for Cornell, she also acted as a cardiology consultant for Sea View Hospital in Staten Island. Travell accepted a Josiah Macy, Jr. Fellowship at Beth Israel Hospital in New York to study arterial disease from 1939 to 1941. It was during her tenure that she first became interested in skeletal muscle pain, which defined her later career. Her research produced new anesthetic techniques for the treatment of painful back muscle spasms that proved very successful among patients. Travell’s techniques included the use of a local procaine injection and vapocoolant sprays to relieve pain. The sprays are still popular in sports medicine treatments today. It was her success with alleviating skeletal muscle pain that resulted in Travell being the first female personal Physician to the President. Travell was called upon by the personal orthopedic surgeon of Senator John F. Kennedy to assist with back pain treatments. Kennedy suffered from terrible pain possibly resulting from invasive back surgeries related to injuries sustained during World War II. When Kennedy won the presidential election in 1960, he appointed her as his personal physician.[2] Her treatments included the use of a rocking chair with a matching rocking ottoman to help alleviate back pain, in the process popularizing their use among the public, who saw the President pictured in his rocker in the Oval Office.[3] She continued to serve as Personal Physician to the President following the assassination of John F. Kennedy, with his successor Lyndon B. Johnson. She continued through Johnson’s re-election, but decided to leave the White House in 1965. While serving as the President’s personal physician, Travell also took on the role of Associate Clinical Professor of Medicine at the George Washington University in 1961. Even after leaving the White House, she continued teaching at the university as a faculty for the School of Medicine. She occupied positions as Associate Clinical Professor 1961–1970, Emeritus Clinical Professor of Medicine 1970–1988, and Honorary Clinical Professor of Medicine from 1988 until her death in 1997. Travell remained active in the medical field until the end: writing articles, giving lectures, and attending conferences.[4] Research[edit] Her personal interest led her to investigate, explain and expound on the phenomenon of myofascial pain syndrome, secondary to trigger points, first written about in the 1920s by Dr Dudley J. Morton.[5] She drew attention to the role of “Morton’s Toe” and its responsibility for causing physical pain throughout the body. Travell’s research resulted in over 100 scientific articles, as well as the acclaimed 1983 co-authored book with David G. Simons: Myofascial Pain and Dysfunction. The Trigger Point Manual. She also wrote her autobiography, Office Hours: Day and Night, which sheds light on her career and life. Quote[edit] “I have lived in a very special world – a world of love and security; beauty and serenity; opportunity, adventure, and variety; challenge and achievement; and the appreciation of my peers. I have had a sufficiency of everything that I desired and a surfeit of nothing.” Dr. Travell, author’s note to Office Hours: Day and Night, 1968.
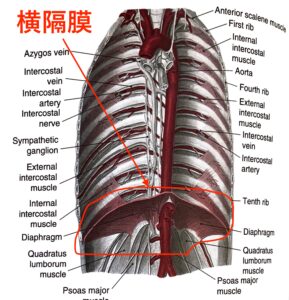
わき腹の痛みを引き起こす横隔膜について

横隔膜っていうのは、いわゆるうすっぺらい膜ではなく、厚みのある筋肉です。イメージしやすいようにかなりくだけた表現で説明すると焼き肉だと、ハラミと言われている部位、ハラミを食べたことある方だとわかりますが、膜ではありませんよね。しっかしとした厚みのある肉です。
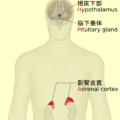
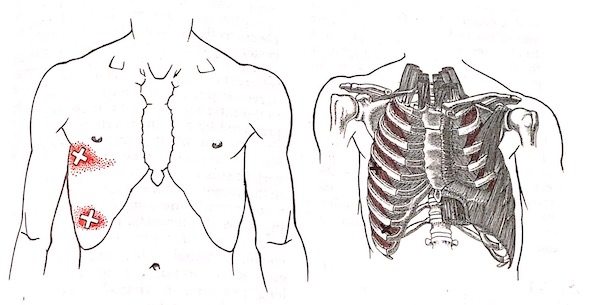
Seventeen patients diagnosed with episodic spasms of the diaphragm complained of chest pain, dyspnea and inability to get a full breath. Sometimes attacks were precipitated by anxiety-producing situations. Patients sometimes had so much difficulty breathing that they feared they might die. This demonstrates the importance of the diaphragm. The author apparently did not consider TrPs, which could account for the symptoms and, if present, would have been a treatable cause. When patients have diaphragmatic TrPs, they are prone to develop a “stitch in the side” when doing exercise that requires rapid deep breaths. The pain is likely to be most intense at the end of a full exhalation when the diaphragm fibers are stretched. Coughing can be excruciatingly painful.
横隔膜の痙攣と診断された17人の患者は胸痛、呼吸困難や深呼吸をすることができないと訴えました。時々、不安感じる状況を作り出すことによって発作が引き起こされました。患者は時々呼吸が非常に困難になり、死ぬのではないかと心配。これは、横隔膜の重要性を示しています。著者は明らかにトリガーポイントを考慮していませんでした。これは症状の原因となる可能性があり、トリガーポイントが存在する場合は治療可能な原因です。 患者が横隔膜のトリガーポイントを持っている場合、急速に深呼吸をしてくださいというと、「側腹筋」の痛みを発症する傾向があります。横隔膜の繊維がストレッチされているとき、完全な呼気の終わりに痛みが最も激しくなる可能性があります。咳は耐え難いほどの痛みを伴うことがあります。

落ち着くために深呼吸して下さいというアドバイスは、横隔膜の筋筋膜痛症候群には、かえって悪影響の可能性があります。


Aさん、今日のブログは、このぐらいにしておきます。急性心筋梗塞・大動脈解離手術後の胸の痛み、パニック障害に似た症状で困っている方があ、少しでも不安な気持ちが和らいでいたら嬉しいです。